 How we found out When I was pregnant I was initially receiving care from my local Midwife team. At my 20 week ultrasound appointment we were told that our baby was a boy, and to go home and enjoy our gender reveal party that night (in hindsight, don't ever schedule a gender reveal party the same day as the ultrasound). Our tech was super sweet, she saw something to be concerned about, but calmly told us to come back next week for some more images that they needed to get. She never led on that something was wrong, I thank her for that grace and allowing us that last cherished, positive moment from my pregnancy. The next week I had a different tech and she paused on the right side of my stomach. They say when you become a Mama your instincts just kick in… it was in that very moment that I just KNEW something wasn’t right. The tech I had that day was, to put it lightly, a moron. She straight up told me “uhhh baby stomach. ummm… no stomach. I need to get the radiologist” and she left me on the table, shirt up, gel on… sobbing uncontrollably in the first of many panic attacks I was yet to experience. Ultrasound technicians are NOT supposed to say ANYTHING. I repeat, they are not supposed to say a damn thing to you. Sometimes in life you just need your mother, and this was 100% one of those times. I am thankful we didn’t clue in to the fact that something was wrong when we want back for those needed images, because my mother came to that appointment instead of my husband. So when I was told that I needed to contact my healthcare team immediately, I had the strongest shoulder in the world that I needed to cry on. Let me tell you, I cried and cried and cried. For us, we caught “something” immediately. Adam’s stomach did not show up in ultrasounds. We know now that it was because it was essentially empty or deflated with nothing inside of it, not that it didn’t exist at all. A lot of EA cases are not discovered before the baby is born, or even until a few days after the baby is born. Each case is so extremely different. I immediately met with my midwives, who had literally no idea what the hell was going on, and who referred me to get genetic testing done, and to a Fetal Medicine Clinic downtown. I had to give up my midwives as my primary caregivers at this point. 
I was induced at 38 weeks due to a condition called Polyhdramnios (pol-e-hi-DRAM-nee-os); the excessive accumulation of amniotic fluid, that happens in 1 to 2 percent of pregnancies. Basically because Adam’s esophagus wasn't connected to his stomach, all of the amniotic fluid couldn’t be swallowed and would end up back into me. I was huge when I was pregnant because of it. When Adam was born he immediately received care from the SickKids team and was then transferred literally across the road (underground) to the Hospital for Sick Children. To be honest, the actual delivery went amazingly, you’re so focused on getting your baby out and into the hands of the doctors to make sure they’re ok. Expect to deliver in the OR instead of your labour and delivery room, with a team full of doctors and specialists, ours were from both Mt. Sinai and SickKids. I don’t know who took over when. Adam was born and they placed him on top of me - something I was not expecting at all. As much as I wanted to hold him, I was practically pushing him away into the hands of the SickKids team to make sure he was ok. They took him into an attached room and we were able to see him before he was transferred across the road to the SickKids NICU. When the baby is born When you see your baby, they will likely be covered in wires and tubes. This is something you will be told, but will never be able to prepare yourself for. I’m sorry, it hurts your heart, but I promise you’ll be able to see past it all at the beauty you’ve created. Adam was born late afternoon, and I was transported by wheelchair to see him that next morning. My husband and mother went with Adam when they took him, my best friend was by my side, and my father stayed with me that night (until I kicked him out for snoring LOL and my Aunt came). It is SO important to have a support system with you. Family, your best friend. You need someone. Physically, emotionally. Someone to bring you a coffee, or a sub, or sushi. Whatever you want - you just gave birth, Mama! But more importantly, someone to hold you when you’re sad, scared, a hot emotional and hormonal mess, because you will be. What you need Rest. You can’t take care of anyone if you’re no good yourself. You’re going to be so damn sore, and exhausted, emotional, anxious. Make sure you’re eating and drinking, and sleeping as much as you can. I say that now - but I fully acknowledge I only slept because of sheer exhaustion. You can’t stay overnight in the NICU. Have a hotel booked close by, you’re going to need to lay down. Mama I can’ stress it enough, you’ve got to heal your body!!! The NICU doctors and nurses are taking care of your baby, there is nothing you can do, but you can take care of the body that grew that sweet babe, you’ve got to. There are no beds in the NICU and often times I was sitting on a stool-type computer chair. This is NO way to heal ANY body after birth, let alone one with an episiotomy or cesarean section. (Adam was birthed vaginally, and yes I had an episiotomy… which didn’t heal properly, surprise - because I was sitting all day every day! Also in part because of the swelling going down and my stitches being loose leaving a gaping hole down there) …now imagine not being able to lay down. You’ve got to get a hotel room, or in with the Ronald McDonald House - which can take a few days, so start that process as soon as possible!!!! I recommend having a suitcase packed with a ton of comfortable clothes. I promise you, everyone looks like hell in the NICU, no one notices those Walmart sweat pants or that favourite slouchy comfy sweater on you. If you don’t know how long you’re going to be there, overpack. You can always keep it in the car. We had our bags packed and ready to go to RMHC because we knew we were in for a longer stay. Once we realized how long we were going to be there (we were originally told more than 3 months at the time, not knowing it would be 8) we had family members drop off a basket of bathroom supplies (bath mat, shower curtain, toothbrush holder, cups) for us to change out at RMH. Though it was a thoughtful and appreciated gesture to make our stay more “homey” with “our stuff”, it was realization that we were going to be there for a long time, like a long ass time. We basically moved in. 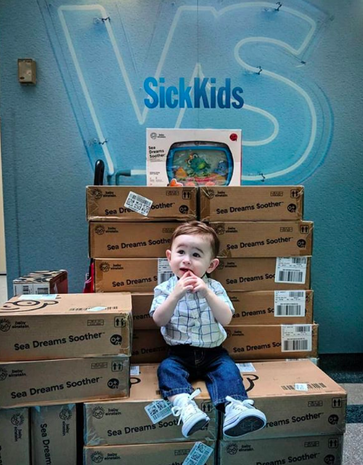 For the hospital, NICU babies don’t wear clothes. Bring your own swaddles and blankets. We had a team of stuffed animals that were special to us that lived at the end of Adam’s bed. We brought a mobile for him to look at, and we were graciously lent a crib side fish tank for him to look at in awe every night when we had to leave. Throughout that stay our crib side fish tank came with us. We gave back the one in the NICU and were able to use our own from home. We were shocked to find out that not every crib had it’s own fish tank as there wasn’t enough to go around. So when we came home, we donated 70 crib side fish tanks not only to the NICU so that EVERY bed could have one, but also to the rest of the hospital as well, so that no baby would ever be without one during their stay. This is one less thing that YOU will have to worry about. Medical procedures Jessica’s section on this topic is different from mine, and from any other patient in a NICU. With each medical case complex and differing, first and foremost it is important for you to acknowledge and ask questions from and to your baby’s medical team. Doctors and specialists can be nerve-wracking to talk to, especially so early on, so feel free to have a trusted or well-liked nurse around to “translate” so to speak. Jessica talks about NG tubes on her side of things. Adam didn’t have one. He was nourished through IV for the first few days of his life and then had a G-Tube placed. The “gastrostomy tube (also called a G-tube) is a tube inserted through the belly that brings nutrition directly to the stomach.” It was Adam’s first procedure and one of our most stressful, because we were entirely new to this world, everything was scary and unknown.  G-Tube: The G-Tube was hands down one of the best things for Adam and for us. We were told that because of the size of his stomach, it would take them longer than usual to insert it, expect 2-3 hours. Adam’s G-Tube was inserted in 45 minutes and they said it was one of the easiest they’ve ever done. HOW? I have no freaking idea. For us, that was the first of many positive tests and procedures to come back. Adam’s G-Tube allowed him to get my pumped breast milk directly into his stomach. They were able to control the speed and the amount and thus resulted in him growing perfectly average - a term that is AMAZING to hear when you live in a hospital. Adam was never on any medication, but when we got home, we would frequently use the g-tube port to directly administer meds like tylenol as well, trust me, you’ll be thankful for it when you go home. The nurses give you lots of practice and hands-on experience to become a pro at your child’s G-Tube. It is required to complete a g-tube course before you leave. Do it. You will become so familiar with it, you’ll be confident and able to teach others. There are some amazing companies out there now that make cute little SkipHop animal backpacks for you to carry around your child’s feeding pump in, on the go. I’ll touch upon that in a future post or podcast.  replogle: Adam had one thing that was constant with us during his stay pre-surgery at the hospital, which is also well-known to every EA baby. A replogle (ree-po-gul). The replogle tube basically goes in one nostril and sits in the pouch where the esophagus ends to suck out secretions. Without it, EA babies will choke and/ or aspirate. Adam needed his replogle to live. He had one until the moment of his surgery. In the NICU the replogle went into Adam’s mouth. When we got up to the General Surgery wing (where we lived for 6+ months) they transferred it to his nose, where it stayed in his right nostril. In most babies, the nurses switch sides when they replace the replogle with a new one when it gets too gummed up. Replogles are often flushed with saline water. Parents are able to flush their baby’s replogle once they are trained and used to doing so. In addition to “flushing” EA babies also need to be “suctioned”. The replogle is constantly connected to a suction mechanism in the wall that keeps the secretions moving. If and when you go for walks around the unit or hallways, you must take a mobile suction unit with you. You CAN go for walks, you just need to ask, go with a nurse at first, and make sure you’re comfortable doing so. The replogle and suction are an EA baby’s literal lifeline before their surgery. PICC line: Jessica mentioned a PICC line. Adam never needed a PICC, he got his meds through his G-Tube. In preparation for his surgery however, they did put one in. It was a horrible experience for us. We were not educated about it, we did not know what it was, we literally went with it because we trusted our nursing and surgical staff. Keep in mind, Adam literally only had his replogle and g-tube for the first 6 months, with zero meds or complications - we were essentially there for his esophagus to grow while he was attached to the suction with his replogle. As Jess mentioned, the PICC line is necessary, and is a regular part of the process. When they tell you what it is and how it’s done… it’s terrifying as a parent, but just know that this is super common and so many babies, children, and adults even have them. Intubation: Intubation for me is a terribly emotional and traumatic topic. Perhaps one I will touch upon in more detail a bit later if I am able to do so. Adam was intubated after his surgery, in the ICU. Nothing in this world, no words, no images, no past experiences can ever prepare you for seeing your baby with a tube down his throat, completely immobile. The sounds of the machine, and the corresponding visuals of your baby’s chest moving up and down, their lungs inflating and deflating with air solely because of this piece of equipment allowing them to do so. Your child is breathing because of a machine. Adam’s lung was collapsed purposely due to surgery. He was completely immobilized afterwards to allow for healing, the intubation was part of the process. We did not see it happen, however we were there when it was taken out. There are personal, private details about struggles we’ve had with Adam being intubated. The tube being cleared, the (wrong) choice to ween him off of a med the night before (resulting in narcotic withdrawal) and delaying the extubation. Also resulting in pneumonia, and our otherwise perfectly healthy baby boy now having seriously threatening issues for the first time in an already hostile situation. There are details… and I can’t talk about them yet. Even just saying what I have already has made me upset and I need to take a break. I will say though, we were given the option to be in the room while they were taking OUT the breathing tube. I’m glad that I was there, I’ll say that. Could I have been there when they put it in? Doubtful, I would have lost my shit 100%. However, when they took it out - I don’t know why I needed to be there, maybe to make sure it happened (even though I couldn’t do anything about it) because I needed to be there if it didn’t work, or if something went wrong? (which it wouldn’t because they do this all the time) …I don’t know why I was there. I lived in that ICU for two week straight, literally did not leave Adam’s side (not exaggerating), so I sure as hell wasn’t leaving when my baby boy was going to be breathing on his own again. Living in a hospital
We lived at SickKids (and RMHC) for just about 3/4 of a year. It is something that you will never get used to, but you will adapt to. Life becomes routine, and a lot of the time your body functions on auto-pilot day to day. Many days are a blur (thankfully they were uneventful for us). I developed OCD (obsessive compulsive disorder) while we lived there. I understand now, after numerous discussions with a therapist that this was my way of coping and holding on to any little bit of control in a chaotic world where I felt that I had no say or control in anything. Counting steps, walking over certain cracks, looking at the exact same thing every single time you walk past it, is a way to gain control over little things that aren't going to change - that you can count on to be present and the same every single time you do it. I recognized this behaviour early on and often made jokes about it to my husband who was experiencing similar things. For example, every night that we walked back to RMH there was a backlit skeleton in one of the windows of the Black Wing… every night my husband and I would say hello to this skeleton, he even had a name that we gave him. We used to walk on the same side of the road, step over the same cracks, look at the same donor name on the wall of RMH (because we associated that company with a very good friend of ours). Every morning I’d start going down the steps with my left foot and count them in my head, pausing if someone said Hi on the way up. I’d look at the same Bravery Bead on the little girl’s picture on the wall, hold my head down in a certain area in the hall. Little things that became my way of coping and making it through my morning, knowing that the day before I did the exact same things and we had a good day. I felt that if I didn’t do these things, it would somehow change how my day was going to go. I understand that that is the OCD talking and that it really has nothing to do with anything, but I felt it. I wasn’t hurting anyone, and it was bringing me peace so I did it. I did it every damn day. It is what it is. You may notice that you develop habits like this if you’re in for an extended stay at the hospital. You may notice that you’re upset more, or anxious. Perhaps you’re scared or angry. All of these feelings are valid. Look at where you are and what you’re exposed to, not just with your child, but the people around you. You’re living in a literal Hell. No one is blaming you for how you’re feeling, you’re absolutely entitled to feel this way and worse, or better, or even nothing at all. Please know that I get it. I understand it. Talk to someone. Reach out to a family member, a friend, a nurse even, a therapist. SickKids has Social Workers who are amazing, genuine, kind, caring people who are there to help you. Contact other parents and support groups. THIS is why we are doing this - because we get it. If you are here and reading this, it’s because you’ve been exposed to or are experiencing a legitimate trauma. It is trauma, it is valid, no matter how long you’ve been in those walls. We are here for you, we understand the highs, lows, in-betweens. I said hello, daily, to a freakin’ skeleton in a window… trust me, you’re not alone in your feelings. You do what you need to do to survive your stay there, no matter how long or short it is.
0 Comments
|
To navigate the BTB blog, you can scroll through the posts, or if you're looking for something specific - you can click on a category below & it will take you to related posts!
••• k Archives
September 2022
Categories
All
|
 RSS Feed
RSS Feed