 With both pregnancies, I received prenatal care at the High-Risk Clinic at Mount Sinai Hospital in Toronto. Once my sons were born, they were immediately attended to by a Sick Kids team working remotely out of Mount Sinai. The team worked until they were stable and then they were directly transferred to the Hospital for Sick Children. Mount Sinai Hospital and the Hospital for Sick Children are world renowned hospitals. The reputations, as well as the team’s working with my family, made me feel 100% at ease. The hospitals work collaboratively to provide frequent meetings for families. The meetings included both the Mount Sinai OBs and a Sick Kids team to explain the plan, what to expect, and answer any questions or fears I had. At the time I was terrified but felt as prepared as I could be. Now that I’ve gone through the experience, I believe that knowledge is power. The more you know going into a difficult situation, the better coping may be. Since I’ve beaten the perceived impossible odd and had two babies with Gastrochisis, I believe that my story can help fully prepare families with what to expect. As mentioned in my intro, the hardest part for me was - and sometimes still is - the feeling of loneliness. This guide is solely based on my experiences and any medical explanations are from my perspective. The purpose of sharing these points is to help parents become ready and aware for the, sometimes very difficult, journey ahead of them. Below I’ve lists factors that I believe are important know. That said, I want to point out that both my children’s conditions were complex and were not a typical Gastrochisis cases. In fact, it was explained to my husband and I that Theo, our first born, was one of the worst cases of Gastrochisis Sick Kids has ever seen. His first surgery was at 4 hours old and my husband was told he may not survive the surgery. I am noting this grim point because my boys went through the worst of it, and now they’re healthy and thriving. Remember, you will get through this:  What to expect and what helped me get though it:
What helped me get through it: Having my spouse or a family member come with me. Despite having such thorough care, being pregnant with a sick baby is terrifying! I know how hard it is for a spouse to take so much time off from work, but you don’t have to go through this alone. Reach out to others. And if no one can come with you physically, tell a loved one when your appointments are and have them check in on you. Consider a FaceTime after the ultrasound or have someone come over for dinner the evening of. Also - SNACKS! Oh man, when you think you have packed enough, add at least 2 more foods to your food bag and 1 more drink! Some appointments were terribly long. Bring something to keep you mind off your appointment other than your phone. Examples include, a book, magazines, downloaded shows, etc. The internet connection wasn’t the greatest, so tangible distractions were helpful. 2. Expect: You may be a complete basket case when the baby is born What most people don’t realize in a Gastrochisis pregnancy is that women are able to have a vaginal birth. Keep in mind, this does depend on your hospital. Since I was being cared for by Mount Sinai and The Hospital for Sick Children, they had specialized staff who can readily handle complex births. If you live in an area where a team needs to be coordinated, you may have a planned c-section. Also, when having a baby with Gastrochisis, you are induced at 37 weeks. Being induced isn’t fun to say the least, but it wasn’t as bad as I thought. There are two ways a woman can be induced. One with a gel and the second is with a foley catheter. For me, the gel was much more pleasant. My experience with the foley catheter was very painful, so if you have the option go for the gel! As well, it was explained to me that if an average healthy pregnancy were to be induced at 37 weeks, most babies would go into distress and need an emergency C-section. But for Gastrochisis babies, they are able to be born vaginally due to an increase in amniotic fluid.  Literally right answer I gave birth to Christian Literally right answer I gave birth to Christian For both my births, I had the OB team and Sick Kids team in the surgical room. This means A LOT of doctors, so be prepared to leave your pride at the door because a whole lot of people are going to be looking at your vagina. Once the baby comes out, you may have a quick peek at your new pride and joy and then the baby will be taken to the adjacent room where the pediatric team will get them stable. Once stable, I was able to have a quick visit with them and then they were taken to Sick Kids. Once YOU are somewhat stable, a transport team take you over in a wheelchair to see your baby. Having a baby under normal circumstances is emotional, but when you’re seeing your baby for the first time and they’re in critical state it can be overwhelming to say the least. Then to see your babe stable but covered with wires and tubes is a whirlwind of emotions. I was happy, I was scared, I was exhausted, I was physically in a lot of pain, and I had so many questions but could not get the words out. I wasn’t able to hold either of my boys for weeks. Something that I am slowly starting to share with others is that I didn’t feel a connection to either of my boys when they were first born. I’ve discovered that this was a coping mechanism. I believe that if my baby died, at least I wasn’t bonded with him. YES, this is some dark and scary shit! But it’s important to be honest and open up about my experience in the hopes of helping others. What helped me get through it: Have people come see you! With Theo (my eldest) I didn’t want anyone at the hospital as I thought it was weird to have visitors with an NICU baby. For me this was not a joyous and exciting time, I was terrified and felt so ripped off of my experience. However, the second time around, when I had Christian, I planned for my sister to be with me as soon as he came out so my husband could immediately go to Sick Kids with the baby. The first time, my dad - God bless him - was the only around during my episiotomy…blah! I’m extremely close with my sister and she is able to make anything into a joke. Her support and help after the birth was comforting and put me in a positive headspace. I recommend having a family member or friend there to support BOTH parents. No matter how much you prepare yourself for this moment, you never know how you will react until you’re in it. And remember, no reaction is right or wrong. Be kind to yourself and don’t forget that this too shall pass… 3. Expect: Not to pack a transitional hospital bag. There is so much information out there on how to pack the “perfect” hospital bag. But this looks very different when having a sick baby. What helped me get through it: STOP following mommy blogs, magazines for mommies to be, etc. Most healthy pregnancy experiences are much different than what I experienced. By removing the comparison of what I thought having a baby would be like was extremely helpful for me. Things you need to pack: For both babies, I stayed at the Ronald McDonald House in Toronto. Sometimes you get in immediately and other times you need to wait - depending on the availability of the house. Both times, my husband and I packed a month’s supply of comfy clothing and personal care items that we left in the car.
Items for my baby: The first time around, I was very upset as the hospital bag I had packed for my baby wasn’t helpful or useful. I couldn’t use anything I packed in the bag and I believe this further increased my disconnection with the baby. As well, not to discredit any of my amazing family or friends, but many generous gifts we were given to us in the hospital so they couldn’t be used. Instead of gifts bringing new parents joy, many gifts added to an already very stressful situation as we couldn’t use most items. The second time around, I thought very hard about what items I could use right away.
 Christian's first outfit put on my mama <3 Christian's first outfit put on my mama <3 4. Baby’s first outfit Unfortunately, I had a pretty negative experience with my eldest son, Theo, regarding his first outfit. To date, I have great relationships with many of the incredible nurses who cared for my boys. We often communicate over social media and I love staying connected with them. When you are in the hospital for such a long time, your nurses not only become your friends but feel like family. Like all situations in life, you’re not going to become friends and like everyone you meet and work with, so of course this was true with our nurses. Once Theo’s intestines were in his stomach, it didn’t occur to me to bring clothes to the hospital to dress him in. For two months prior, he was just in a diaper and wearing socks and a hat. Like many new moms, I had a special outfit picked out for him that I had hoped to dress him in it. I came to the hospital one morning and a nurse (one who I did not have a good relationship with) had dressed him in used hospital clothing. Her intentions were in the right place and honestly if another nurse dressed him, I probably wouldn’t have been so upset. However, when you’re already had issues conceiving, followed by a complex pregnancy and then a critically ill child, you feel you have been robbed of so much. This was something I was greatly looking forward to and I was devastated to see my baby dressed, not only by someone I did not like but on top of that, in used hospital clothes. Something you CAN do: The second time around I explained my past experience to a nurse I had a close relationship with. She validated my experience and suggested that I hang Christian’s outfit on the side of the crib. At the beginning, I didn’t want to do it as I was still really upset about my last experience. But hanging the outfit and seeing it there daily ended up being a positive thing for me. It gave me hope that Christian would soon be healthy, and I would be able to hold him in the near future. It also helped me feel like a mom and that I was somewhat in control of my situation. I highly recommend still bringing your baby’s first outfit along with the hanger and having it near the isolate (an isolate is like an incubator as it keeps the baby warm, but they’re not completely covered).  Items to have nearby:
5. Medical procedures that will probably happen: As I mentioned in this section, Mount Sinai and Sick Kids work together and set up meetings with in hopes of preparing parents prior to having their sick baby. From going through my experience TWICE, the NICU is all I know. During this difficult time, transparence is key. I believe if I was prepared more with the ugly truth of what to really expect, perhaps the first time around, our experience may have been less traumatic. In my opinion, the best way to fight fear is with information. When reading through this list remember that most medical procedures that happen on your baby are completely terrifying. But if you are expecting them to take place, then they may be less overwhelming. I was prepared for the ugly reality of the NICU the second time around and procedures were far less daunting, as I expected them and knew they were part of the process. How the heck does their intestines go back in? Once your beautiful babe comes out, a pediatric team will immediately start to care for your baby in a separate room. In my case, the room was attached to the delivery room. You will see your baby once they’re stable from the birth and the intestines are cleaned. When I saw my eldest, I remember thinking he looked like a mummy from ancient Egypt - his stomach was completely rapped up with white gauze. Your baby with also have an IV started and an NG tube, which will be explained later. Obviously, this is probably not the idea you had in mind when you found out you were expecting. To be honest, this part wasn’t as scary as I thought it would be. Everything was so surreal; I don’t know how, but I just went with the motions. [Note: to this day, I still struggle when seeing pictures of new mom’s holding their babies. I don’t think I will ever enjoy a Pampers commercial and I can feel my stomach turn when I hear positive labour stories. I am no longer angry about my story, but I think I will always be sad that I could not hold by baby for so long…and I’m learning that these feelings that have stuck with me are valid]Once your baby is safe to transfer, they will be taken to Sick Kids. Now their intestines will look different. Typically, the intestines are in a clear bag attached to a string, which is then attached to a C shaped bar that anchors overs your baby’s isolate. This allows for gravity to start making room for the intestines to descend into the stomach. Our eldest son’s case was very complicated, and his intestines were in bad shape when he was born. During his treatment, a surgical nurse showed me a picture of what his intestines looked like immediately after birth and it was grotesque! The intestines enter the body in 3 steps: 1) Gravity: as the baby is laying of its back, gravity encourages the intestines to naturally descend into the stomach. 2) Reductions: the surgical team would come by every couple of days and depending on how the baby is doing, they would slowly squeeze the bag or push down on the intestines. This is quick but can be painful and for this reason babies are given pain medication. 3) Surgery: Once the intestines are very close to the stomach wall, they will bring surgically stitched back together. Pictures: In recent years, I only started sharing pictures of my babies’ condition. I used to be terrified of other people these pictures. I imagined them sharing them to their friends and family as if they were a learning exhibit. But now, I believe it is extremely important to show images of what this condition really could look like. Parents need to understand and prepare themselves for what to expect. For me, I saw a picture of a baby with their intestines in a bag at the high-risk clinic at Mount Sinai Hospital. Even though it was only one picture, and it was quite dated, I found it very helpful. Not only seeing the typical size of the baby (both boys were approximately 5.5 lbs) it was helpful for me to visualize what it looks like to have a baby with intestines outside their body. Even NOW posting these pictures I have NEVER shared until now, bring tears to my eyes....  NG-Tube Once your baby is born, they will immediately have an NG tube placed on the inside of their mouth or nose. Because their intestines are outside the body, the NG tube helps to remove all the bile/waste out. To this day it breaks my heart when I see a Sick Kids advertisement showing a baby with my NG tube. As I will talk about later, Theo, had a lot of problems with feeding and had an NG tube for some time. Christian, our second child, only had it for the first two months at the hospital and did awesome at feeding once it was removed. Once the tube is placed inside your little babe, rest assured that they usually are quite comfortable. Seeing the tube go in that can be quite distressing. Remember most kiddos will only have the tube for a short period of time. PICC A couple days after Theo was born, we were told they would need a PICC. A what???? It was explained to me that this is a long-term IV that helps the baby directly get the nutrients. Your baby will not eat until their intestines are inside their body and once they are inside, they will very slowly start to drink breastmilk through either a NG tube, breast and or bottle. There are two ways a baby can have a PICC placed inside them. It can be done by a specialized nurse in the NICU or alternatively, the baby can be taken down to IGT where a paediatric radiologist uses diagnostic imaging to guide the PICC into place. For either procedures, your baby will be sedated. When we were first told that Theo would need a PICC we were completely terrified about the procedure and honestly, I thought he would die having it done. At the time, this procedure seemed extremely scary and daunting. However, once the PICC has been placed, it’s actually a great thing because it reduces the amount of times a baby is getting poked with an IV. With a PICC, doctors will have IV access and therefore need far less poking. The second time around, it was not stressful as we were prepared for this step and knew it was part of the process. We also asked and advocated for Christian to get a PICC immediately to reduce IV poking. Blood transfusion: Babies often need blood, especially before surgery to top up their hemoglobin as a precautionary measure. I’m not sure about you but, prior to this experience, when I heard “blood transfusion” I automatically thought someone was dying and they needed blood to live. I actually once said that to a nurse, and she laughed because it was such an inaccurate explanation of why babies need blood in the NICU. As mentioned prior, Theo‘s recovery in the hospital was very rocky. The first week he was doing well, as his intestine slowly were placed back into his stomach but then the second week, he developed NIC and E.coli in his blood. Not only were his intestines extremely dilated but these infections were life-threatening. One day we got a call at around 3am that Theo needed blood. It was one of the scariest nights as we didn’t know what state he would be in when we got to the hospital. Seeing a very pale sick baby being pumped with blood is terrifying, even if it is only a precautionary measure. A beautiful thing happened in our NICU room. As most people are aware, The Hospital for Sick Children is in the process of building a new hospital. The current NICU is extremely tight space. There is tape on the floor around your baby’s crib to indicate your space, so there is very little privacy between you and other families. That said, being in such close proximity to other people in the same situation as you can sometimes be a blessing. When Theo was hooked up with blood and quite critical, we started talking to the parents next to us. The mom said, “I know it’s scary to have blood hooked-up to your baby but honestly they do it all the time here.” She told me that her baby already had three transfusions. I remember looking at her like she was speaking another language but having her reassurance that this was part of the process was so comforting. Needless to say, it was an automatic friendship that we still have today. Intubation Intubation is when a breathing tube is placed down your baby’s throat and into their lungs to help them breathe. I’m going to be brutally honest with you; this is something very hard to prepare for. Babies, particularly babies with Gastro, need to be intubated because as their intestines are slowly pressed into their stomach so this puts a lot of pressure on the lungs and makes it difficult to breathe. Also, since the intestines are slowly being pushed into the stomach, your baby will be on a higher dose of pain medication which sometimes makes the lungs “lazy” and impacts breathing. Theo was intubated and extubated several times, but Christian was fully intubated for six weeks. The second time around, when Cristian was intubated, we were called and told it was going to happening. I anticipated this step in the process, but it was still hard to hear. Although Christian was in a much better situation then Theo, my husband started bawling when he heard the news. I can remember the call from in our nurse practitioner like it was yesterday. When your baby is intubated, they try to keep them as comfortable as possible but it’s still very hard to see. Despite this process being incredibly hard to deal with, I think it’s important to know that this is expected and needed in order for your baby to recover. I would like to make a side note about intubation; as mentioned prior, we had some touch and go moments with Theo. There was a situation where he needed to be intubated rather quickly. At this time, my husband and I were given the option to stay in the room. I understand why the option is given to parents, however, after going through the distressful situation I truly believe parents should not be allowed to stay in the room. I have advocated this to the NICU and understand it is a divided issue. I strongly advise any parent to remove yourself from the room during this procedure. The nurses, RT’s and doctors are experts. They know what they’re doing. They know that baby will look distressed during this process and they know the perfect steps of securing the breathing tube in place. During this procedure, my husband and I were both crying, and I ran out of the room and threw up. Breathing tube insertion are not fun. Once they’re in though, they are somewhat manageable to deal with.
0 Comments
 How we found out When I was pregnant I was initially receiving care from my local Midwife team. At my 20 week ultrasound appointment we were told that our baby was a boy, and to go home and enjoy our gender reveal party that night (in hindsight, don't ever schedule a gender reveal party the same day as the ultrasound). Our tech was super sweet, she saw something to be concerned about, but calmly told us to come back next week for some more images that they needed to get. She never led on that something was wrong, I thank her for that grace and allowing us that last cherished, positive moment from my pregnancy. The next week I had a different tech and she paused on the right side of my stomach. They say when you become a Mama your instincts just kick in… it was in that very moment that I just KNEW something wasn’t right. The tech I had that day was, to put it lightly, a moron. She straight up told me “uhhh baby stomach. ummm… no stomach. I need to get the radiologist” and she left me on the table, shirt up, gel on… sobbing uncontrollably in the first of many panic attacks I was yet to experience. Ultrasound technicians are NOT supposed to say ANYTHING. I repeat, they are not supposed to say a damn thing to you. Sometimes in life you just need your mother, and this was 100% one of those times. I am thankful we didn’t clue in to the fact that something was wrong when we want back for those needed images, because my mother came to that appointment instead of my husband. So when I was told that I needed to contact my healthcare team immediately, I had the strongest shoulder in the world that I needed to cry on. Let me tell you, I cried and cried and cried. For us, we caught “something” immediately. Adam’s stomach did not show up in ultrasounds. We know now that it was because it was essentially empty or deflated with nothing inside of it, not that it didn’t exist at all. A lot of EA cases are not discovered before the baby is born, or even until a few days after the baby is born. Each case is so extremely different. I immediately met with my midwives, who had literally no idea what the hell was going on, and who referred me to get genetic testing done, and to a Fetal Medicine Clinic downtown. I had to give up my midwives as my primary caregivers at this point. 
I was induced at 38 weeks due to a condition called Polyhdramnios (pol-e-hi-DRAM-nee-os); the excessive accumulation of amniotic fluid, that happens in 1 to 2 percent of pregnancies. Basically because Adam’s esophagus wasn't connected to his stomach, all of the amniotic fluid couldn’t be swallowed and would end up back into me. I was huge when I was pregnant because of it. When Adam was born he immediately received care from the SickKids team and was then transferred literally across the road (underground) to the Hospital for Sick Children. To be honest, the actual delivery went amazingly, you’re so focused on getting your baby out and into the hands of the doctors to make sure they’re ok. Expect to deliver in the OR instead of your labour and delivery room, with a team full of doctors and specialists, ours were from both Mt. Sinai and SickKids. I don’t know who took over when. Adam was born and they placed him on top of me - something I was not expecting at all. As much as I wanted to hold him, I was practically pushing him away into the hands of the SickKids team to make sure he was ok. They took him into an attached room and we were able to see him before he was transferred across the road to the SickKids NICU. When the baby is born When you see your baby, they will likely be covered in wires and tubes. This is something you will be told, but will never be able to prepare yourself for. I’m sorry, it hurts your heart, but I promise you’ll be able to see past it all at the beauty you’ve created. Adam was born late afternoon, and I was transported by wheelchair to see him that next morning. My husband and mother went with Adam when they took him, my best friend was by my side, and my father stayed with me that night (until I kicked him out for snoring LOL and my Aunt came). It is SO important to have a support system with you. Family, your best friend. You need someone. Physically, emotionally. Someone to bring you a coffee, or a sub, or sushi. Whatever you want - you just gave birth, Mama! But more importantly, someone to hold you when you’re sad, scared, a hot emotional and hormonal mess, because you will be. What you need Rest. You can’t take care of anyone if you’re no good yourself. You’re going to be so damn sore, and exhausted, emotional, anxious. Make sure you’re eating and drinking, and sleeping as much as you can. I say that now - but I fully acknowledge I only slept because of sheer exhaustion. You can’t stay overnight in the NICU. Have a hotel booked close by, you’re going to need to lay down. Mama I can’ stress it enough, you’ve got to heal your body!!! The NICU doctors and nurses are taking care of your baby, there is nothing you can do, but you can take care of the body that grew that sweet babe, you’ve got to. There are no beds in the NICU and often times I was sitting on a stool-type computer chair. This is NO way to heal ANY body after birth, let alone one with an episiotomy or cesarean section. (Adam was birthed vaginally, and yes I had an episiotomy… which didn’t heal properly, surprise - because I was sitting all day every day! Also in part because of the swelling going down and my stitches being loose leaving a gaping hole down there) …now imagine not being able to lay down. You’ve got to get a hotel room, or in with the Ronald McDonald House - which can take a few days, so start that process as soon as possible!!!! I recommend having a suitcase packed with a ton of comfortable clothes. I promise you, everyone looks like hell in the NICU, no one notices those Walmart sweat pants or that favourite slouchy comfy sweater on you. If you don’t know how long you’re going to be there, overpack. You can always keep it in the car. We had our bags packed and ready to go to RMHC because we knew we were in for a longer stay. Once we realized how long we were going to be there (we were originally told more than 3 months at the time, not knowing it would be 8) we had family members drop off a basket of bathroom supplies (bath mat, shower curtain, toothbrush holder, cups) for us to change out at RMH. Though it was a thoughtful and appreciated gesture to make our stay more “homey” with “our stuff”, it was realization that we were going to be there for a long time, like a long ass time. We basically moved in. 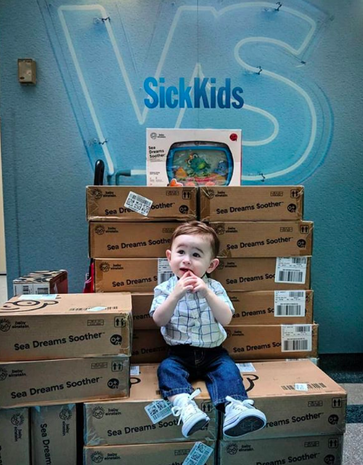 For the hospital, NICU babies don’t wear clothes. Bring your own swaddles and blankets. We had a team of stuffed animals that were special to us that lived at the end of Adam’s bed. We brought a mobile for him to look at, and we were graciously lent a crib side fish tank for him to look at in awe every night when we had to leave. Throughout that stay our crib side fish tank came with us. We gave back the one in the NICU and were able to use our own from home. We were shocked to find out that not every crib had it’s own fish tank as there wasn’t enough to go around. So when we came home, we donated 70 crib side fish tanks not only to the NICU so that EVERY bed could have one, but also to the rest of the hospital as well, so that no baby would ever be without one during their stay. This is one less thing that YOU will have to worry about. Medical procedures Jessica’s section on this topic is different from mine, and from any other patient in a NICU. With each medical case complex and differing, first and foremost it is important for you to acknowledge and ask questions from and to your baby’s medical team. Doctors and specialists can be nerve-wracking to talk to, especially so early on, so feel free to have a trusted or well-liked nurse around to “translate” so to speak. Jessica talks about NG tubes on her side of things. Adam didn’t have one. He was nourished through IV for the first few days of his life and then had a G-Tube placed. The “gastrostomy tube (also called a G-tube) is a tube inserted through the belly that brings nutrition directly to the stomach.” It was Adam’s first procedure and one of our most stressful, because we were entirely new to this world, everything was scary and unknown.  G-Tube: The G-Tube was hands down one of the best things for Adam and for us. We were told that because of the size of his stomach, it would take them longer than usual to insert it, expect 2-3 hours. Adam’s G-Tube was inserted in 45 minutes and they said it was one of the easiest they’ve ever done. HOW? I have no freaking idea. For us, that was the first of many positive tests and procedures to come back. Adam’s G-Tube allowed him to get my pumped breast milk directly into his stomach. They were able to control the speed and the amount and thus resulted in him growing perfectly average - a term that is AMAZING to hear when you live in a hospital. Adam was never on any medication, but when we got home, we would frequently use the g-tube port to directly administer meds like tylenol as well, trust me, you’ll be thankful for it when you go home. The nurses give you lots of practice and hands-on experience to become a pro at your child’s G-Tube. It is required to complete a g-tube course before you leave. Do it. You will become so familiar with it, you’ll be confident and able to teach others. There are some amazing companies out there now that make cute little SkipHop animal backpacks for you to carry around your child’s feeding pump in, on the go. I’ll touch upon that in a future post or podcast.  replogle: Adam had one thing that was constant with us during his stay pre-surgery at the hospital, which is also well-known to every EA baby. A replogle (ree-po-gul). The replogle tube basically goes in one nostril and sits in the pouch where the esophagus ends to suck out secretions. Without it, EA babies will choke and/ or aspirate. Adam needed his replogle to live. He had one until the moment of his surgery. In the NICU the replogle went into Adam’s mouth. When we got up to the General Surgery wing (where we lived for 6+ months) they transferred it to his nose, where it stayed in his right nostril. In most babies, the nurses switch sides when they replace the replogle with a new one when it gets too gummed up. Replogles are often flushed with saline water. Parents are able to flush their baby’s replogle once they are trained and used to doing so. In addition to “flushing” EA babies also need to be “suctioned”. The replogle is constantly connected to a suction mechanism in the wall that keeps the secretions moving. If and when you go for walks around the unit or hallways, you must take a mobile suction unit with you. You CAN go for walks, you just need to ask, go with a nurse at first, and make sure you’re comfortable doing so. The replogle and suction are an EA baby’s literal lifeline before their surgery. PICC line: Jessica mentioned a PICC line. Adam never needed a PICC, he got his meds through his G-Tube. In preparation for his surgery however, they did put one in. It was a horrible experience for us. We were not educated about it, we did not know what it was, we literally went with it because we trusted our nursing and surgical staff. Keep in mind, Adam literally only had his replogle and g-tube for the first 6 months, with zero meds or complications - we were essentially there for his esophagus to grow while he was attached to the suction with his replogle. As Jess mentioned, the PICC line is necessary, and is a regular part of the process. When they tell you what it is and how it’s done… it’s terrifying as a parent, but just know that this is super common and so many babies, children, and adults even have them. Intubation: Intubation for me is a terribly emotional and traumatic topic. Perhaps one I will touch upon in more detail a bit later if I am able to do so. Adam was intubated after his surgery, in the ICU. Nothing in this world, no words, no images, no past experiences can ever prepare you for seeing your baby with a tube down his throat, completely immobile. The sounds of the machine, and the corresponding visuals of your baby’s chest moving up and down, their lungs inflating and deflating with air solely because of this piece of equipment allowing them to do so. Your child is breathing because of a machine. Adam’s lung was collapsed purposely due to surgery. He was completely immobilized afterwards to allow for healing, the intubation was part of the process. We did not see it happen, however we were there when it was taken out. There are personal, private details about struggles we’ve had with Adam being intubated. The tube being cleared, the (wrong) choice to ween him off of a med the night before (resulting in narcotic withdrawal) and delaying the extubation. Also resulting in pneumonia, and our otherwise perfectly healthy baby boy now having seriously threatening issues for the first time in an already hostile situation. There are details… and I can’t talk about them yet. Even just saying what I have already has made me upset and I need to take a break. I will say though, we were given the option to be in the room while they were taking OUT the breathing tube. I’m glad that I was there, I’ll say that. Could I have been there when they put it in? Doubtful, I would have lost my shit 100%. However, when they took it out - I don’t know why I needed to be there, maybe to make sure it happened (even though I couldn’t do anything about it) because I needed to be there if it didn’t work, or if something went wrong? (which it wouldn’t because they do this all the time) …I don’t know why I was there. I lived in that ICU for two week straight, literally did not leave Adam’s side (not exaggerating), so I sure as hell wasn’t leaving when my baby boy was going to be breathing on his own again. Living in a hospital
We lived at SickKids (and RMHC) for just about 3/4 of a year. It is something that you will never get used to, but you will adapt to. Life becomes routine, and a lot of the time your body functions on auto-pilot day to day. Many days are a blur (thankfully they were uneventful for us). I developed OCD (obsessive compulsive disorder) while we lived there. I understand now, after numerous discussions with a therapist that this was my way of coping and holding on to any little bit of control in a chaotic world where I felt that I had no say or control in anything. Counting steps, walking over certain cracks, looking at the exact same thing every single time you walk past it, is a way to gain control over little things that aren't going to change - that you can count on to be present and the same every single time you do it. I recognized this behaviour early on and often made jokes about it to my husband who was experiencing similar things. For example, every night that we walked back to RMH there was a backlit skeleton in one of the windows of the Black Wing… every night my husband and I would say hello to this skeleton, he even had a name that we gave him. We used to walk on the same side of the road, step over the same cracks, look at the same donor name on the wall of RMH (because we associated that company with a very good friend of ours). Every morning I’d start going down the steps with my left foot and count them in my head, pausing if someone said Hi on the way up. I’d look at the same Bravery Bead on the little girl’s picture on the wall, hold my head down in a certain area in the hall. Little things that became my way of coping and making it through my morning, knowing that the day before I did the exact same things and we had a good day. I felt that if I didn’t do these things, it would somehow change how my day was going to go. I understand that that is the OCD talking and that it really has nothing to do with anything, but I felt it. I wasn’t hurting anyone, and it was bringing me peace so I did it. I did it every damn day. It is what it is. You may notice that you develop habits like this if you’re in for an extended stay at the hospital. You may notice that you’re upset more, or anxious. Perhaps you’re scared or angry. All of these feelings are valid. Look at where you are and what you’re exposed to, not just with your child, but the people around you. You’re living in a literal Hell. No one is blaming you for how you’re feeling, you’re absolutely entitled to feel this way and worse, or better, or even nothing at all. Please know that I get it. I understand it. Talk to someone. Reach out to a family member, a friend, a nurse even, a therapist. SickKids has Social Workers who are amazing, genuine, kind, caring people who are there to help you. Contact other parents and support groups. THIS is why we are doing this - because we get it. If you are here and reading this, it’s because you’ve been exposed to or are experiencing a legitimate trauma. It is trauma, it is valid, no matter how long you’ve been in those walls. We are here for you, we understand the highs, lows, in-betweens. I said hello, daily, to a freakin’ skeleton in a window… trust me, you’re not alone in your feelings. You do what you need to do to survive your stay there, no matter how long or short it is. |
To navigate the BTB blog, you can scroll through the posts, or if you're looking for something specific - you can click on a category below & it will take you to related posts!
••• k Archives
September 2022
Categories
All
|









 RSS Feed
RSS Feed